Energy modelling of patient pathways
The Conclude Consultancy has recently completed a fascinating study into the energy modelling of patient pathways. We believe that this work will make a significant contribution to understanding how energy is consumed in complex facilities such as acute hospitals. We believe that this will be the case because we have succeeded in directly correlating the energy impacts of use to each patient episode within any part of the hospital.
Why is this important?
It is important for a number of reasons. Firstly because current norms of energy consumption are usually based on building area and volume. So typical norms are: kWh/m² or GJ/100m³ . Many of the standards used in health care facility energy performance use these norms. Yet they can be both very misleading as well as potentially irrelevant to the needs of a clinician who might just be interested in how they personally or how their department could improve energy consumption. Such norms are misleading because they do not reflect intensity of use. For example for the energy conscious clinician when they see that despite the results of their efforts consumption actually goes up, would that not be a little deflating for them? Perhaps the reason for the increase in consumption is because the number of patients processed through the department has risen, and perhaps it is that increase which has caused the increase in consumption? This is what we mean by intensity of use: more patients per hour, per day, per month for example. Perhaps it is the difference of intensity of use between UK hospitals and those in Europe that explains why UK hospitals do not appear to perform as well from an energy consumption perspective?
In Figure 1 we can see (if you click on the image it will enlarge) that France and Finland for example have similar intensity of use, but the evidence is that their acute hospitals appear to perform better than the UK from an energy performance perspective. In contrast Swedish hospitals appear to perform much better than the UK hospitals, but then they have much lower intensity of use. So if intensity of use might partially explain the difference in performance (all supposing we are comparing like for like) then what are the other factors that drive energy consumption and how might these be controlled?
This leads is to the second point as to why area or volume based norms are misleading. It is because of this – that unless the clinicians can be presented with concrete evidence to explain how their working practices impact energy consumption, then they are unlikely to appreciate the need for change. Consequently area or volume based norms mean little to them, because they are intangible measures unrelated to their work. However, by correlating their working practices directly to patient centric energy consumption, then compelling evidence to support the need for change can be provided. We mean by patient centric energy consumption that energy consumption is directly correlated to each patient episode for each patient type. It follows that the energy needs of different patient types will vary according to the demand for clinical services of that patient type. Clearly a patient requiring a video fluoroscopy will consume more energy in their episode than an orthopaedic patient having a plaster cast removed. Furthermore, studies in the United States have demonstrated how different x-ray equipment can impact the working practices of the clinician and yet have very different energy consumption profiles. Both the studies that we have been involved in and the research that we have undertaken have demonstrated much potential for control of energy consumption through analysis of working practices and operational policies. This is the evidence that clinicians require to start to see the need for change.
How did we carry out our analysis?
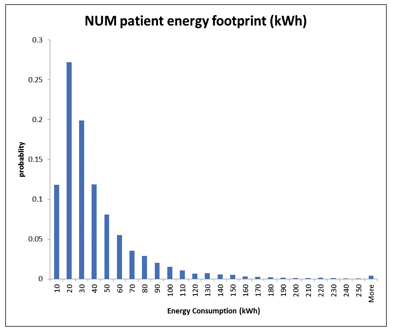
We have developed two forms of analytics: OCCUPANCY ANALYTICS ™ and Whole Facility Energy Modelling. (Please refer to the Conclude Process at the bottom of our web page). By taking a whole systems perspective of organisational processes and energy modelling focused on patient demand, we have been able to understand the impact of working practices and the energy impacts of those practices from different perspectives within the organisation. For example we can study consumption from a whole hospital perspective, but we can also study it from a departmental, or specialist function perspective. Yet we can also study it from a patient perspective. We have been able to achieve this because we understand the statistical probability of where each patient type will be in the hospital at any hour of the day. We also understand the energy consumption within each part of the hospital at each hour of the day, and thus by modelling these two datasets we can forecast the statistical probability of energy consumption for each patient type for each patient episode at any period of the day.
How does this help the clinician to understand how they could influence energy consumption?
Because we use the documented working practices and operational processes as the basis of our simulation (quantitative analysis) and so provide the evidence to explains the impact on energy consumption. We then work with the clinicians to consider ‘what-if’ scenarios where we consider the energy impacts of different working practices and operational policies. We discuss the issues and the challenges and in doing so establish a clear context for improvement (qualitative) analysis. It is through this process that clinicians are empowered through learning – learning about how to they can impact energy consumption – consumption focused on each patient pathway through the organisation.
It is through this learning that clinicians can also start to understand how the control of patient flow impacts energy consumption, because flow impacts the demand on the environmental systems that provide occupant comfort. As flow becomes interrupted it places larger demands on those systems – a demand which drives energy consumption. In Conclude, we argue that if we can improve patient flow – we can also improve energy consumption. In fact we can also impact the sizing of the engineering systems, which drives down the capital cost of them. Effective management of patient flow impacts not just the patient experience (reduced waiting times for example) but improved energy performance.
It is for all of these reasons that modelling of patient pathways offers many benefits, and not just providing visibility to the factors that drive energy consumption. It also becomes a valuable means to bridge the divide between the coupling of hospital engineering design with In-use working practices, and that must be a good thing.
Tweet This
![Intensity of use. [Source: http://www.hope.be]](http://www.conclude.org.uk/wp-content/uploads/2014/03/Intensity-of-use-300x112.jpg)

Follow us
on Twitter